Are you suffering from plantar fasciitis?
By Ryde Natural Health Clinic’s Osteopath – Evan Marnezos
Understanding Plantar Fasciitis
 Plantar fasciitis is a very common cause of heel discomfort that can be debilitatingly painful. Ignoring plantar fasciitis can result in chronic heel pain which interrupts your everyday life. In this article, I will explain what plantar fasciitis is, the symptoms, causes, and how you can properly manage it.
Plantar fasciitis is a very common cause of heel discomfort that can be debilitatingly painful. Ignoring plantar fasciitis can result in chronic heel pain which interrupts your everyday life. In this article, I will explain what plantar fasciitis is, the symptoms, causes, and how you can properly manage it.
What is it?
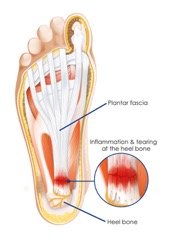
Plantar fasciitis is painful inflammation of a thick band of tissue (fascia) that runs across the bottom the foot, reaching from the heel to the toes. This band of tissue supports the muscles and arch of the foot.
What are the symptoms of plantar fasciitis?
Patients I see often point to a specific location in the heel or foot which causes them pain.
Symptoms of plantar fasciitis include:
– Stabbing pain in the bottom of the foot, usually in the morning which is felt on the first few steps;
– Pain for several days to several months in the heel, mid foot or arch which is constant or recurring;
– Increased pain with initial standing, walking, running which usually improves as activity continues then gets worse at the end of the day or next day.
What causes plantar fasciitis?
The plantar fascia acts as a shock absorbing tissue which supports the foot and functions painlessly. When excessive tension and stress is placed on the plantar fascia it can cause small tears, irritation, and inflammation. This can create pain, and an inflammatory cycle to occur. When the plantar fascia is stuck in this inflammatory cycle, symptoms manifest which often leads to a host of biomechanical problems. These biomechanical problems commonly manifest as knee, hip and/or lower back pain or dysfunction. This often occurs because of other underlying issues in the your body such as abnormal function in your feet, calves, and glutes which leads to the plantar fascia working harder, causing more load and stress on it, in turn leading it to becoming symptomatic.
Plantar fasciitis can occur from:
– Improper footwear
– Prolonged standing with poor foot and ankle biomechanics
– Tight muscles in the ankle/foot/calf
– Abnormal function of foot/ankle/calf/glutes
– Foot structure – high arches as well as flat feet can contribute
– Increase in body weight
How can you and your Osteopath help?
Home treatments like rest, icing, and anti-inflammatory drugs are often the first ways to reduce the symptoms of plantar fasciitis. This will often provide temporary relief however, will not address the cause of your plantar fasciitis. If the cause of the inflammation is not addressed, your plantar fasciitis will often return and can become a chronic condition. This can be a lot harder to properly manage as your plantar fascia becomes ‘stuck’ in a chronic inflammatory cycle.
In order to properly manage your plantar fasciitis, an Osteopath will prioritise different goals at different stages of your recovery. Unloading the plantar fascia to reduce the inflammation, provide symptomatic relief and allow your body’s natural healing process to thrive is the first goal in management and recovery. This includes reducing the tension and strengthening the plantar fascia, calves and ankles through techniques such as joint mobilisation of the feet, soft tissue releases, taping, dry needling, strengthening exercises and trigger point therapy.
Once the plantar fascia has been unloaded and starts healing, correcting the structure and function of the foot is then prioritised as the next goal, to minimise the continual load to the plantar fascia and limit the return of the inflammation. This includes correcting any abnormal structure or function such as flat feet, weak/tight foot muscles, calves, hips, knees and glutes, as well as education on how to properly weight-bare when standing, walking or running on the outer portion of the feet, and correct footwear.
Once the underlying abnormal structure and function of your plantar fasciitis has been addressed, building a sustainable self-management routine will be emphasised by your Osteopath to help reduce any tension from your everyday life accumulating, to help prevent any tightness or pain from coming back. This will be in the form of a simple daily routine involving some stretches and exercises which will be useful to your individual work/home/athletic environment, as well as avoiding certain poor postures or positions that might be harmful to you.
In some cases, conservative management will not be enough to recover from plantar fasciitis.
If conservative measures do not work, it might be recommended by your Osteopath to see your doctor to discuss:
– Corticosteroid injection which can provide temporary relief and reduce inflammation
– Surgery (if pain is severe affecting quality of life after all other options have failed)
Although these options can be beneficial, they do not always give long-term relief and can lead to other issues. It is advised to prevent the need for these more invasive interventions as there is a risk for weakening the arch of the foot, leading to more problems in future.
In summary
Plantar fasciitis can be a painfully limiting condition that can often become worse when unmanaged. Most people recover with Osteopathy, self-management and medical treatments and don’t need surgery to relieve pain. If not properly taken care of, symptoms can persist for years if left unmanaged so be sure to get on top of your plantar fasciitis.
If you find yourself suffering from heel pain that is not getting better on its own, book in to see your Osteopath to get a management plan suitable for you!

